Epidemiology

| For country-level data, see: | |
COVID-19 pandemic by country and territory | |
 Cases
57,974,667 Deaths
1,378,411 As of 21 November 2020 | |
Africa · Asia · Europe · North America Oceania · South America |
Background
Although it is still unknown exactly where the outbreak first started, several early infected people had visited Huanan Seafood Wholesale Market, located in Wuhan, Hubei, China. On 11 February 2020, the World Health Organization (WHO) named the disease "COVID-19", which is short for coronavirus disease 2019. The virus that caused the outbreak is known as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), a newly discovered virus closely related to bat coronaviruses, pangolin coronaviruses, and SARS-CoV. The scientific consensus is that COVID-19 has a natural origin. The probable bat-to-human infection may have been among people processing bat carcasses and guano in the production of traditional Chinese medicines.
The earliest known person with symptoms was later discovered to have fallen ill on 1 December 2019, and that person did not have visible connections with the later wet market cluster. Of the early cluster of cases reported that month, two-thirds were found to have a link with the market. There are several theories about when and where the very first case (the so-called patient zero) originated.
Cases
Official case counts refer to the number of people who have been tested for COVID-19 and whose test has been confirmed positive according to official protocols. Many countries, early on, had official policies to not test those with only mild symptoms. An analysis of the early phase of the outbreak up to 23 January estimated 86 percent of COVID-19 infections had not been detected, and that these undocumented infections were the source for 79 percent of documented cases. Several other studies, using a variety of methods, have estimated that numbers of infections in many countries are likely to be considerably greater than the reported cases.
On 9 April 2020, preliminary results found that 15 percent of people tested in Gangelt, the centre of a major infection cluster in Germany, tested positive for antibodies. Screening for COVID-19 in pregnant women in New York City, and blood donors in the Netherlands, has also found rates of positive antibody tests that may indicate more infections than reported. Seroprevalence based estimates are conservative as some studies shown that persons with mild symptoms do not have detectable antibodies. Some results (such as the Gangelt study) have received substantial press coverage without first passing through peer review.
Analysis by age in China indicates that a relatively low proportion of cases occur in individuals under 20. It was not clear whether this was because young people were less likely to be infected, or less likely to develop serious symptoms and seek medical attention and be tested. A retrospective cohort study in China found that children and adults were just as likely to be infected.
Initial estimates of the basic reproduction number (R0) for COVID-19 in January were between 1.4 and 2.5, but a subsequent analysis concluded that it may be about 5.7 (with a 95 percent confidence interval of 3.8 to 8.9). R0 can vary across populations and is not to be confused with the effective reproduction number (commonly just called R), which takes into account effects such as social distancing and herd immunity. By mid-May 2020, the effective R was close to or below 1.0 in many countries, meaning the spread of the disease in these areas at that time was stable or decreasing.

Epidemic curve of daily new cases of COVID-19 (7 day rolling average) by continent

Semi-log plot of weekly new cases of COVID-19 in the world and top five current countries (mean with deaths)
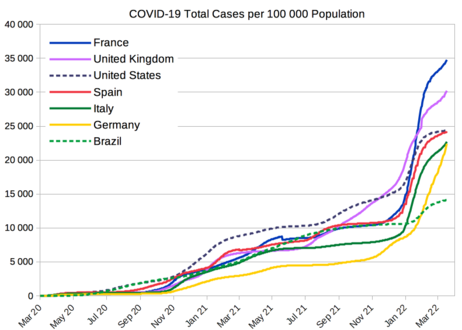
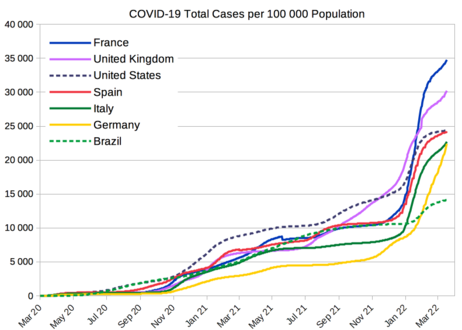
COVID-19 total cases per 100 000 population from selected countries
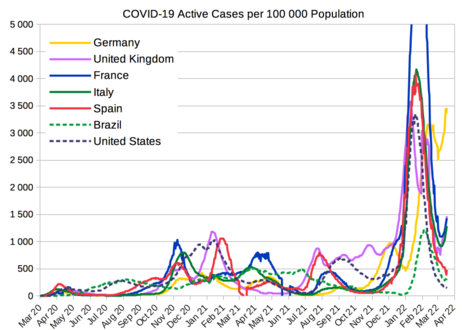
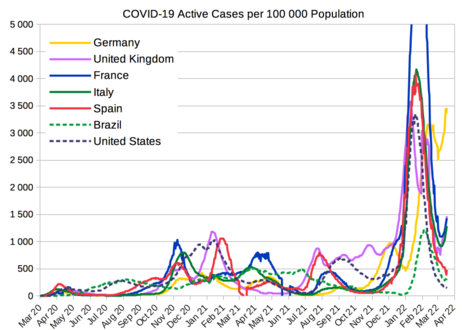
COVID-19 active cases per 100 000 population from selected countries
Deaths
Official deaths from COVID-19 generally refer to people who died after testing positive according to protocols. This may ignore deaths of people who die without having been tested. Conversely, deaths of people who had underlying conditions may lead to over-counting. Comparison of statistics for deaths for all causes versus the seasonal average indicates excess mortality in many countries. This may include deaths due to strained healthcare systems and bans on elective surgery. The first confirmed death was in Wuhan on 9 January 2020. The first reported death outside of China occurred on 1 February in the Philippines, and the first reported death outside Asia was in the United States on 6 February.
More than 95% of the people who contract COVID-19 recover. Otherwise, the time between symptoms onset and death usually ranges from 6 to 41 days, typically about 14 days. As of 21 November 2020, more than 1.37 million deaths had been attributed to COVID-19. People at the greatest risk from COVID-19 tend to be those with underlying conditions, such as a weakened immune system, serious heart or lung problems, severe obesity, or the elderly.
On 24 March 2020, the Centers for Disease Control and Prevention (CDC) of the United States changed the criteria for attributing deaths to COVID-19 to include those marked "probable"/"likely." The CDC said, "It is not likely that the National Center for Health Statistics (NCHS) will follow up on these cases" and that while the "underlying cause depends upon what and where conditions are reported on the death certificate, … the rules for coding and selection of the ... cause of death are expected to result in COVID–19 being the underlying cause more often than not."
On 16 April 2020, the World Health Organization (WHO) created two codes for classifying deaths: UO7.1, "confirmed by laboratory testing irrespective of severity of clinical signs or symptoms"; and UO7.2, "diagnosed clinically or epidemiologically but laboratory testing is inconclusive or not available". The WHO "recognized that in many countries detail as to the laboratory confirmation… will not be reported and recommended, for mortality purposes only, to code COVID-19 provisionally to code U07.1 unless it is stated as 'probable' or 'suspected'." It was also noted that the WHO "does not distinguish" between infection by SARS-CoV-2 and COVID-19.
Multiple measures are used to quantify mortality. These numbers vary by region and over time, influenced by testing volume, healthcare system quality, treatment options, government response, time since the initial outbreak, and population characteristics, such as age, sex, and overall health. Countries like Belgium include deaths from suspected cases of COVID-19, regardless of whether the person was tested, resulting in higher numbers compared to countries that include only test-confirmed cases.
The death-to-case ratio reflects the number of deaths attributed to COVID-19 divided by the number of diagnosed cases within a given time interval. Based on Johns Hopkins University statistics, the global death-to-case ratio is 2.4 percent (1,378,411 deaths for 57,974,667 cases) as of 21 November 2020. The number varies by region.

Semi-log plot of weekly deaths due to COVID-19 in the world and top five current countries (mean with cases)

COVID-19 deaths per 100 000 population from selected countries
Infection fatality ratio (IFR)
The most important metric in assessing death rate is the infection fatality ratio (IFR),c which is deaths attributed to disease divided by individuals infected (including all asymptomatic and undiagnosed) to-date. In March, a peer-reviewed analysis of pre-serology data from mainland China yielded an overall IFR of 0.66% (with age-bracketed values ranging from 0.00161% for 0–9 years to 0.595% for 50–59 years to 7.8% for > 80 years).
In April 2020, an IFR range of 0.12–1.08% was derived from non-peer-reviewed serology surveys, with the upper bound characterized as much more credible and the range indicated as from 3 to 27 times deadlier than influenza (0.04%).
In July 2020, the US CDC adopted the IFR as a "more directly measurable parameter for disease severity for COVID-19" and computed an overall 'best estimate' for planning purposes for the U.S. of 0.65%. In September, the CDC computed an age-bracketed 'best estimate' for the U.S. of 0.003% for 0–19 years; 0.02% for 20–49 years; 0.5% for 50–69 years; and 5.4% for 70+ years.d
In August 2020, the WHO reported serology testing for three locations in Europe (with some data through 2 June) that showed IFR overall estimates converging at approximately 0.5-1%. A systematic review article in The BMJ advised that "caution is warranted … using serological tests for … epidemiological surveillance" and called for higher quality studies assessing accuracy with reference to a standard of "RT-PCR performed on at least two consecutive specimens, and, when feasible, including viral cultures." CEBM researchers have called for in-hospital 'case definition' to record "CT lung findings and associated blood tests" and for the WHO to produce a "protocol to standardise the use and interpretation of PCR" with continuous re-calibration.
| Coronavirus |
|---|
 |
|
Types
|
|
Diseases
|
|
Vaccines
|
|
Outbreaks, epidemics, and pandemics
|
|
See also
|
In September 2020, a Bulletin of the World Health Organization article by John Ioannidis estimated global IFR inferred from seroprevalence data at 0.23%e overall and 0.05% for people < 70 years, much lower than estimates made earlier in the pandemic. Ioannides criticized prior "average IFR … irresponsibly circulated widely in media and social media" as "probably extremely flawed as they depended on erroneous modeling assumptions, and/or focused only on selecting mostly studies from countries high death burden (that indeed have higher IFRs), and/or were done by inexperienced authors who used overtly wrong meta-analysis methods in a situation where there is extreme between-study heterogeneity. As the data for his analysis was drawn "predominantly from hard-hit epicenters", Ioannides indicates that even lower "average values of 0.15–0.25% … and 0.03–0.04% for <70 years) as of October 2020 are plausible." He also notes that in European countries with a large numbers of cases and deaths and in the U.S., "many, and in many cases most, deaths occurred in nursing homes".
On 6 October 2020, Dr. Mike Ryan, director of the WHO's Health Emergencies Programme announced "Our current best estimates tell us that about 10% of the global population may have been infected by this virus." Also in October, the Centre for Evidence-Based Medicine (CEBM) reported a 'presumed estimate' of global IFR at between 0.10% to 0.35%, noting that this will vary between populations due to differences in demographics. These researchers noted a decrease in IFR in England over time;f and, for the UK and Italy (the two Europeans nations worst hit by COVID-19), attribute the rise in daily cases, stability in daily deaths, and shift of cases to a younger population to waning viral circulation, misapplication of testing, and misinterpretation of test results rather than to prevention, treatment, or virus mutation.
Case fatality ratio (CFR)
Another metric in assessing death rate is the case fatality ratio (CFR),g which is deaths attributed to disease divided by individuals diagnosed to-date. This metric can be misleading because of the delay between symptom onset and death and because testing focuses on individuals with symptoms (and particularly on those manifesting more severe symptoms). On 4 August, WHO indicated "at this early stage of the pandemic, most estimates of fatality ratios have been based on cases detected through surveillance and calculated using crude methods, giving rise to widely variable estimates of CFR by country – from less than 0.1% to over 25%."




Comments
Post a Comment